by Nathan Favini, MD, MS, Forward Medical Lead, and Richard B. Lanman, MD, Forward Advisor
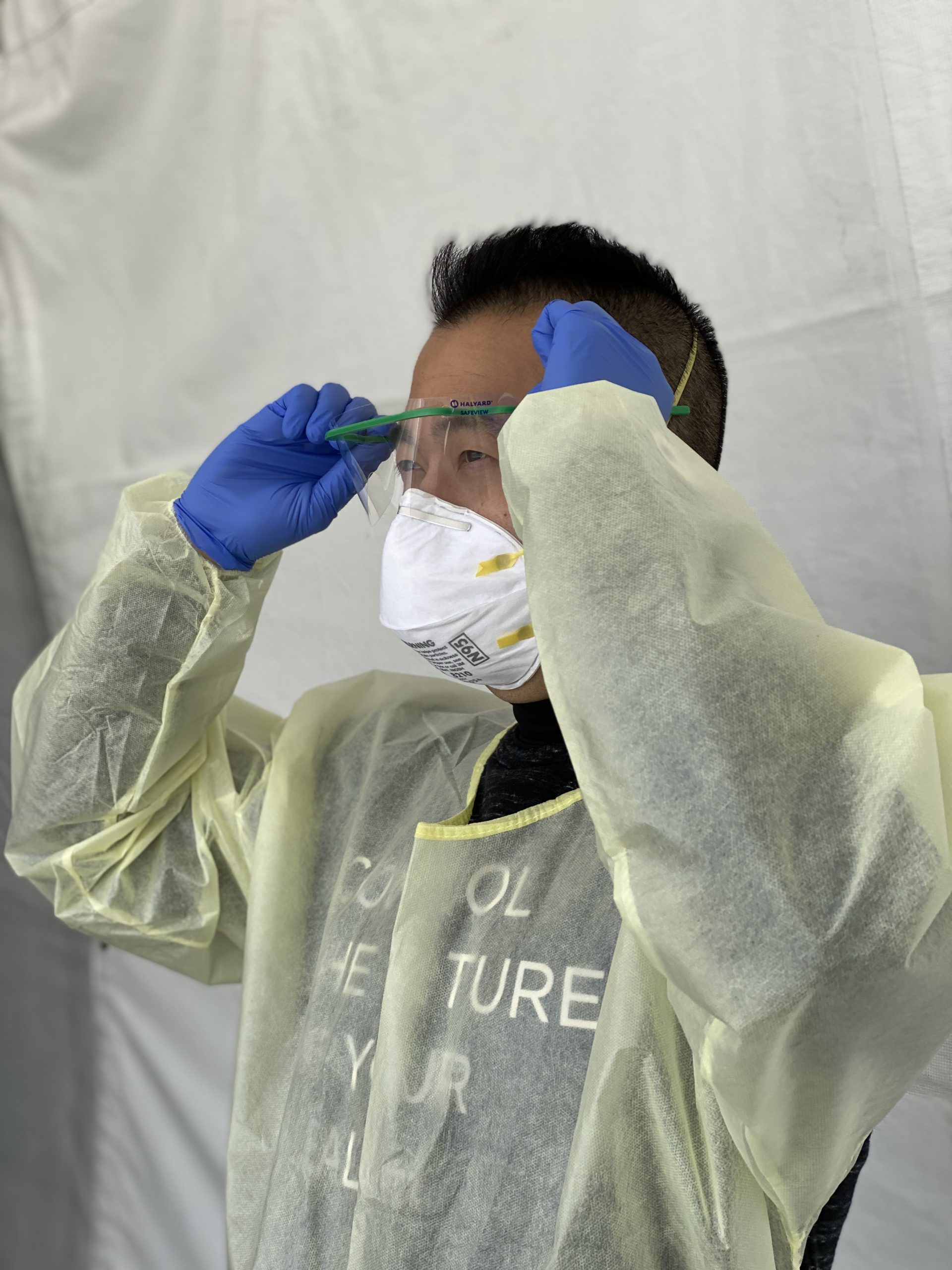
Following the news about the state of COVID-19 testing can be confusing. Every day we see articles about new types of testing, yet most people have limited access to testing of any kind, and those that do have access may have questions about the validity of the results. We‘ll break down the two primary types of tests, their uses, limitations and how we decide what’s best when caring for our members. We value shared decision-making at Forward, so here’s some transparency into our process.
RT-PCR Test
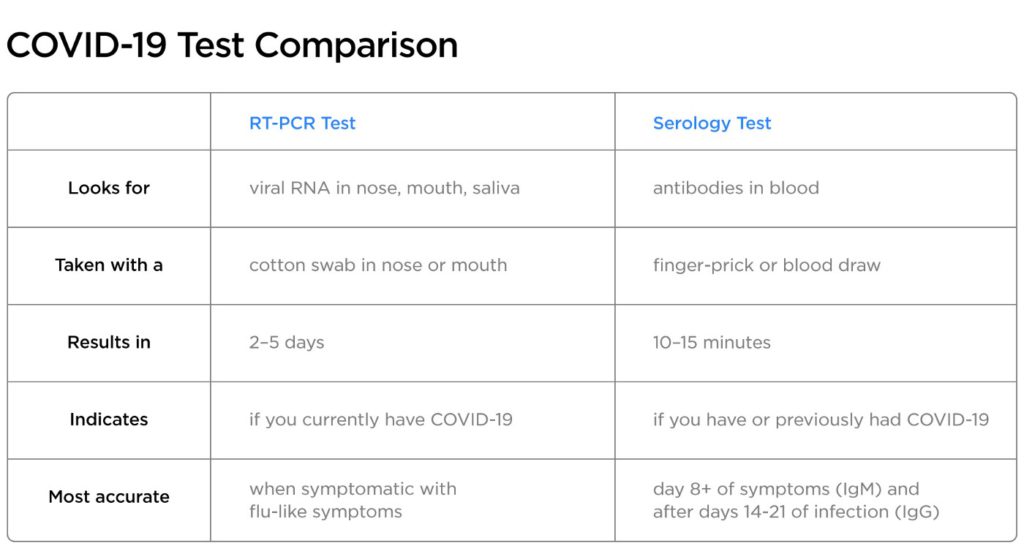
The first type uses a method known as RT-PCR (short for reverse transcriptase polymerase chain reaction), which looks for the presence of viral RNA. RT-PCR, or just PCR for short, can be run on samples from your nose, mouth and, in some cases, from saliva. The samples currently need to be processed in reference laboratories, and results take between two to five days on average to return. The FDA has recently authorized faster, point-of-care PCR tests, but they are not yet widely available.
Serology (Antibody) Test
The second type is serology testing. These tests look for two types of antibodies that are produced by your body in response to the SARS-CoV-2 virus, which causes COVID-19. This test is performed on a single drop of blood, often obtained by a simple finger-prick. These tests produce results in just 10–15 minutes and can indicate if you have or previously had COVID-19. Importantly, they have a higher risk of producing a false-positive result than PCR-tests and should not be used to infer that someone has immunity against the coronavirus. Forward is currently validating the performance characteristics of multiple brands of antibody tests by using them in conjunction with PCR testing for our members.
The timing of your symptoms can help your Care Team decide which test is best for you.
Symptomatic
COVID-19 symptoms tend to develop two to-14 days after exposure to the virus, with symptoms developing by five days after exposure in 50% of cases. As symptoms develop, the viral RNA load rises in the nasopharynx or saliva and is most detectable while you are symptomatic. The best way to assess your symptoms is to use the COVID-19 assessment tool (in app for members or free online COVID-19 risk assessment for non-members). Concerning symptoms include cough, fever, shortness of breath, loss of smell or taste and body aches. Contact with someone who has COVID-19 and being an essential worker can both increase the likelihood that you may have COVID-19 as well. At Forward, we recommend PCR testing for people that have had flu-like symptoms for seven days or less, when the viral RNA load is most detectable.
Day 8 to Symptom Resolution
As the virus progresses, your body creates antibodies to fight COVID-19. Immunoglobin M (IgM) is generally detectable after 7 days of symptoms. At Forward, we recommend serology testing in combination with PCR for people that have had symptoms for longer than seven days because they likely have detectable levels of both IgM antibodies and viral RNA. We also offer PCR testing to symptomatic members in this phase of the illness.
Post Symptom Resolution
After 14 days of symptoms, viral RNA and IgM antibodies will generally be waning. However, the second antibody, Immunoglobin G (IgG), slowly increases and becomes detectable after 14 days. These antibodies remain in the blood even after a person has recovered from COVID-19. We don’t know how long a person has antibodies for (in a study of SARS and MERS IgG antibodies remained elevated for two to three years) or to what degree they confer immunity, so everyone should continue following safe distancing regardless of serology results. At Forward, we recommend serology tests for people who had symptom onset more than 14 days ago and whose symptoms have resolved, because there is a good chance that IgG will be detected.
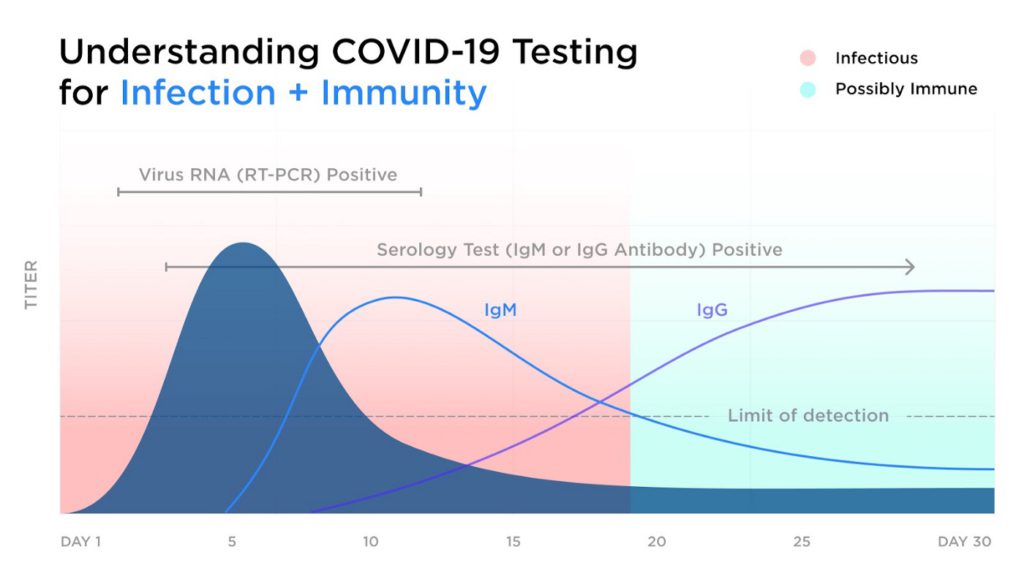
If serology testing is negative in members with COVID-19 symptoms, PCR testing should be conducted to make sure that COVID-19 infection was not missed. Today, we conduct confirmatory PCR tests in addition to antibody tests.
Current rapid antibody tests have a higher risk of false-positive results than PCR tests because other proteins in your blood may appear like coronavirus antibodies. This is another reason to use PCR testing to confirm certain serology test results, when positive. Serology testing is not only useful for diagnosis in symptomatic persons, it is also a valuable tool for identifying who had asymptomatic prior infections. However, these qualitative serology tests cannot determine to what degree antibodies provide immunity to COVID-19 or how long immunity lasts. Forward is closely following the science of immunity and advances in antibody testing, so that we can offer immunity assessments when they are scientifically validated. For now, everyone, regardless of results indicating past infection, should continue to follow safe distancing, frequent hand washing suggestions, cleaning frequently touched surfaces, and wearing surgical masks in crowded places.
Dr. Nate Favini is Medical Lead at Forward, the preventive primary care practice combining top-rated doctors and advanced medical technology. Dr. Richard B. Lanman has an extensive career at the intersection of health and innovation, most recently serving as Chief Medical Officer of Guardant Health and is a Medical Advisor at Forward. Forward’s COVID-19 Care Program helps you stay on top of new information as the state of the pandemic changes. We now offer the COVID vaccine, as well as COVID treatment, prevention, and symptom assessments to help you stay ahead of the virus.